Frozen Shoulder
Definition
Permanent severe
limitation of the range of motion of the shoulder due to inflammation and
subsequent scarring around the shoulder joint (adhesive capsulitis) . Frozen
shoulder may occur following an injury or immobilization of the shoulder joint,
and it occurs more commonly in people with diabetes and certain other health
conditions than in the general population.
Anatomy
The shoulder joint is formed where the
humerus (upper arm bone) fits into the scapula (shoulder blade), like a ball
and socket. Other important bones in the shoulder include, the acromion is a
bony projection off the scapula. The clavicle (collarbone) meets the acromion
in the acromioclavicular joint. The coracoid process is a hook-like bony
projection from the scapula. The shoulder has several other important structures,
the rotator cuff is a collection of muscles and tendons that surround the
shoulder, giving it support and allowing a wide range of motion. The bursa is a
small sac of fluid that cushions and protects the tendons of the rotator cuff.
A cuff of cartilage called the labrum forms a cup for the ball-like head of the
humerus to fit into. The humerus fits relatively loosely into the shoulder
joint. This gives the shoulder a wide range of motion, but also makes it
vulnerable to injury.
The rotator cuff is a group of tendons and
muscles in the shoulder, connecting the upper arm (humerus) to the shoulder
blade (scapula). The rotator cuff tendons provide stability to the shoulder,
the muscles allow the shoulder to rotate. The muscles in the rotator cuff include,
Teres minor, Infraspinatus, Supraspinatus, Subscapularis. Each muscle of the
rotator cuff inserts at the scapula, and has a tendon that attaches to the
humerus. Together, the tendons and other tissues form a cuff around the
humerus.
Pathophysiology
Frozen shoulder can be classified by two
that is Primary and secondary frozen shoulder. Primary frozen shoulder is cause
by diabetes mellitus (both insulin-dependent and non-insulin-dependent types), especially retinopathy, but exists also with
hypo- and hyperthyroidism. Dupuytren’s disease is shown to be related to frozen
shoulder, Dupuytren’s disease is significantly more common than usual among
male relatives to frozen shoulder and
the microscopic changes in the anterior capsule and coracohumeral ligament are
very similar to those in Dupuytren’s disease of the hand, Similarities with
Dupuytren’s are shown when analysing the fibrotic capsule for cytokines and
proteinases. There is an involvement of the capsule in the glenohumeral joint. The capsule volume is reduced and this is the
cause for the restricted range of motion, look arthroscopically in the joint is
technically more difficult than in a normal shoulder. The dense capsule is difficult to penetrate
and the tight joint with marked reduced volume is demanding to visualise
without compromising the joint surfaces.
The capsule is tight and its synovial surface is showing signs of
vascular inflammation. Usually, no intra
articular adhesions are seen.
For Secondary frozen shoulder the cause of
the syndrome is usually easy to define. In the posttraumatic cases there is
clear evidence of a trauma and usually also structural changes within or
adjacent to the joint, such as fractures, chondral lesions, avascular necrosis
or tendon injuries. Scarring following
traumatic tissue injury is another cause. The iatrogenic cases occur following
treatment, usually surgery. In these
cases extreme scarring following tissue repair may occur or surgical mistakes
such as over tightening of soft tissue may be responsible for the following
limitation in range of movement.
The pattern in which frozen shoulder usually is
developed may be described as three time periods of six months each, 1st
period(Freezing). The freezing stage shows an insidious onset where pain is
dominating the clinical picture. Quite
often, subacromial impingement is initially suspected because of the
involvement of the subacromial bursa. At
the end of this period range of motion becomes limited in the typical way and
diagnosis is usually no longer a problem. 2nd period(Frozen). The frozen period
shows reduction of pain but the restricted mobility remains.3rd
period(Thawing). The thawing includes successive reestablishment of normal or
near normal range of motion.
Causes
Frozen shoulder
can develop when you stop using the joint normally because of pain, injury, or
a chronic health condition, such as diabetes or a stroke. Any shoulder problem
can lead to frozen shoulder if you do not work to keep full range of motion.
Frozen shoulder occurs, after surgery or injury, most often in people 40 to 70
years old, more often in women (especially in postmenopausal women) than in
men, most often in people with chronic diseases.
Sign and symptoms
Movement of the shoulder
is severely restricted, with progressive loss of both active and passive range
of motion. The condition is sometimes caused by injury, leading to lack of use
due to pain, but also often arises spontaneously with no obvious preceding
trigger factor (idiopathic frozen shoulder). Rheumatic disease progression and
recent shoulder surgery can also cause a pattern of pain and limitation similar
to frozen shoulder. Intermittent periods of use may cause inflammation.
In frozen shoulder, there is a lack of
synovial fluid, which normally helps the shoulder joint, a ball and socket
joint, move by lubricating the gap between the humerus (upper arm bone) and the
socket in the shoulder blade. The shoulder capsule thickens, swells, and
tightens due to bands of scar tissue (adhesions) that have formed inside the
capsule. As a result, there is less room in the joint for the humerus, making
movement of the shoulder stiff and painful. This restricted space between the
capsule and ball of the humerus distinguishes adhesive capsulitis from a less
complicated, painful, stiff shoulder.
People with diabetes, stroke, lung disease,
rheumatoid arthritis, or heart disease are at a higher risk for frozen
shoulder. Injury or surgery to the shoulder or arm may cause the capsule to
tighten from reduced use during recovery. Adhesive capsulitis has been
indicated as a possible adverse effect of some forms of highly active
antiretroviral therapy (HAART).
The condition rarely appears in people under
40 years old and, at least in its idiopathic form, is much more common in women
than in men (70% of patients are women aged 40–60). Frozen shoulder in diabetic
patients is generally thought to be a more troublesome condition than in the
non-diabetic population, and the recovery is longer.Cases have also been reported
after breast and lung surgery
Doctor management
Physical Examination, after discussing your
symptoms and medical history, your doctor will examine your shoulder. Your
doctor will move your shoulder carefully in all directions to see if movement is
limited and if pain occurs with the motion. The range of motion when someone
else moves your shoulder is called "passive range of motion." Your
doctor will compare this to the range of motion you display when you move your
shoulder on your own ("active range of motion"). People with frozen
shoulder have limited range of motion both actively and passively.Imaging
Tests, other tests that may help your doctor rule out other causes of stiffness
and pain include, X-rays. Dense structures, such as bone, show up clearly on
x-rays. X-rays may show other problems in your shoulder, such as arthritis.
Magnetic resonance imaging (MRI) and ultrasound. These studies can create
better images of problems with soft tissues, such as a torn rotator cuff.
Non-steroidal anti-inflammatory medicines. Drugs like aspirin and ibuprofen
reduce pain and swelling. Steroid injections. Cortisone is a powerful
anti-inflammatory medicine that is injected directly into your shoulder
joint.Surgical Treatment, if your symptoms are not relieved by therapy and
anti-inflammatory medicines, you and your doctor may discuss surgery. It is
important to talk with your doctor about your potential for recovery continuing
with simple treatments, and the risks involved with surgery.The goal of surgery
for frozen shoulder is to stretch and release the stiffened joint capsule. The
most common methods include manipulation under anesthesia and shoulder
arthroscopy.
Physiotherapy management
Modalities
Modalities, such as hot packs, can be applied
before or during treatment. Moist heat used in conjunction with stretching can
help to improve muscle extensibility and range of motion by reducing muscle
viscosity and neuromuscular-mediated relaxation. Patients improved with
combined therapy which involved hot and cold packs applied before and after
shoulder exercises were performed. However,
ultrasound, massage, iontophoresis, and phonophoresis reduced the odds
of improved outcomes for patients with adhesive capsulitis.
Initial Phase
As stated previously, treatment should be
customized to each individual based on what stage or phase of adhesive
capsulitis they are in.Pain relief should be the focus of the initial phase,
also known as the Painful, Freezing Phase. During this time, any activities
that cause pain should be avoided and pain-free activities should be allowed.
Better results have been found in patients who performed pain-free exercise,
rather than intensive physical therapy. In patients with high irritability,
range of motion exercises performed with low intensity and a short duration can
alter joint receptor input, reduce pain, and decrease muscle guarding.
Stretches may be held from one to five seconds at a pain-free range, two to
three times a day. A pulley may be used to assist range of motion and stretch,
depending on the patient’s ability to tolerate the exercise. Core exercises
include pendulum exercise, passive supine forward elevation, passive external
rotation with the arm in approximately forty degrees of abduction in the plane
of the scapula, and active assisted range of motion in extension, horizontal
adduction, and internal rotation. Positional stretching of the coracohumeral
ligament was performed for a patient in the first phase of adhesive capsulitis.
The patient's Disabilities of Arm Shoulder and Hand (DASH) scores improved from
65 to 36 and Shoulder Pain and Disability Index (SPADI) scores improved from 72
to 8 and passive external rotation from 20 degrees to 71 degrees.
The stretches performed focused on providing
positional low load and prolonged stretch to the CHL and the area of the
rotator interval capsule following anatomical fiber orientation. The rationale
behind this was to produce tissue remodeling through gentle and prolonged
tensile stress on the restricting tissues. While a cause and effect
relationship cannot be inferred from a single case, this report may help with
further investigation regarding therapeutic strategies to improve function and
reduce loss of range of motion in the shoulder and the role that the CHL plays
in this. In the case of adhesive capsulitis, physical therapy can also be a
complement to other therapies (such as steroid injections as discussed
previously), especially to improve the range of motion of the shoulder.
Concominant exercises to steroid injections included isometric strengthening in
all ranges once motion was reached in 90% of normal ranges, theraband exercises
in all planes, scapular stabilization exercises, and later, advanced muscular
strengthening with dumbbells.
Second Phase
During the adhesive phase, the focus of
treatment should be shifted towards more aggressive stretching exercises in
order to improve range of motion. The patient should perform low load,
prolonged stretches in order to produce plastic elongation of tissues and avoid
high load, brief stretches, which would produce high tensile resistance.
Demonstrated success of a non-operative treatment through a four-direction
shoulder stretching exercise program in which 90% of the patients reported a
satisfactory outcome. During the second phase of treatment, movement with
mobilization and end range mobilization have shown to be successful, according
to a randomized multiple treatment . In this trial, the patients had
statistically significant improvements in the Flexi-Level Scale of Shoulder
Function (FLEX-SF), arm elevation, scapulohumeral rhythm, humeral external
rotation, and humeral internal rotation. Mobilization with movement also
corrected scapulohumeral rhythm significantly better than end range
mobilization did. The goal for end range mobilization was not only to restore
joint play, but also to stretch contracted periarticular structures, whereas
the goal for mobilization with movement was to restore pain-free motion to the
joints that had painful limitation of range of motion. Showed that physical
therapy paired with dynamic splinting had better outcomes compared to physical
therapy alone or dynamic splinting alone. The patients in this group of
combined treatments received physical therapy twice a week and a Shoulder Dynasplint
System (SDS) for daily end-range stretching. Methods for this treatment include
moist heat, patient education and re-evaluation of symptoms, joint mobilization
(limited to progressive end-range joint mobilization), passive range of motion,
active range of motion and PNF, and therapeutic exercise. The SDS was worn
twice each day for seven days per week and was set at for the first week in order to allow the
patient to accommodate to the stretching. After accommodation, the setting was
increased to, which equals three foot lbs of force. The progression of the
stretch as well as the adjustment for pain or soreness was standardized, and
instructions were given to the patient to follow accordingly. Patients were
instructed to increase the duration in the SDS unit for 20 – 30 minutes twice
each day (with the intention to stretch 60 minutes each day. The combination of
physical therapy with dynamic splinting had significant improvements in active,
external rotation in patients with adhesive capsulitis.
Third Phase
During stage three, also known as the
Resolution Phase, treatment is progressed primarily by increasing stretch
frequency and duration, while maintaining the same intensity, as the patient is
able to tolerate. The stretch can be held for longer periods, and the sessions
per day can be increased. As the patient’s irritability level becomes low, more
intense stretching and exercises using a device, such as a
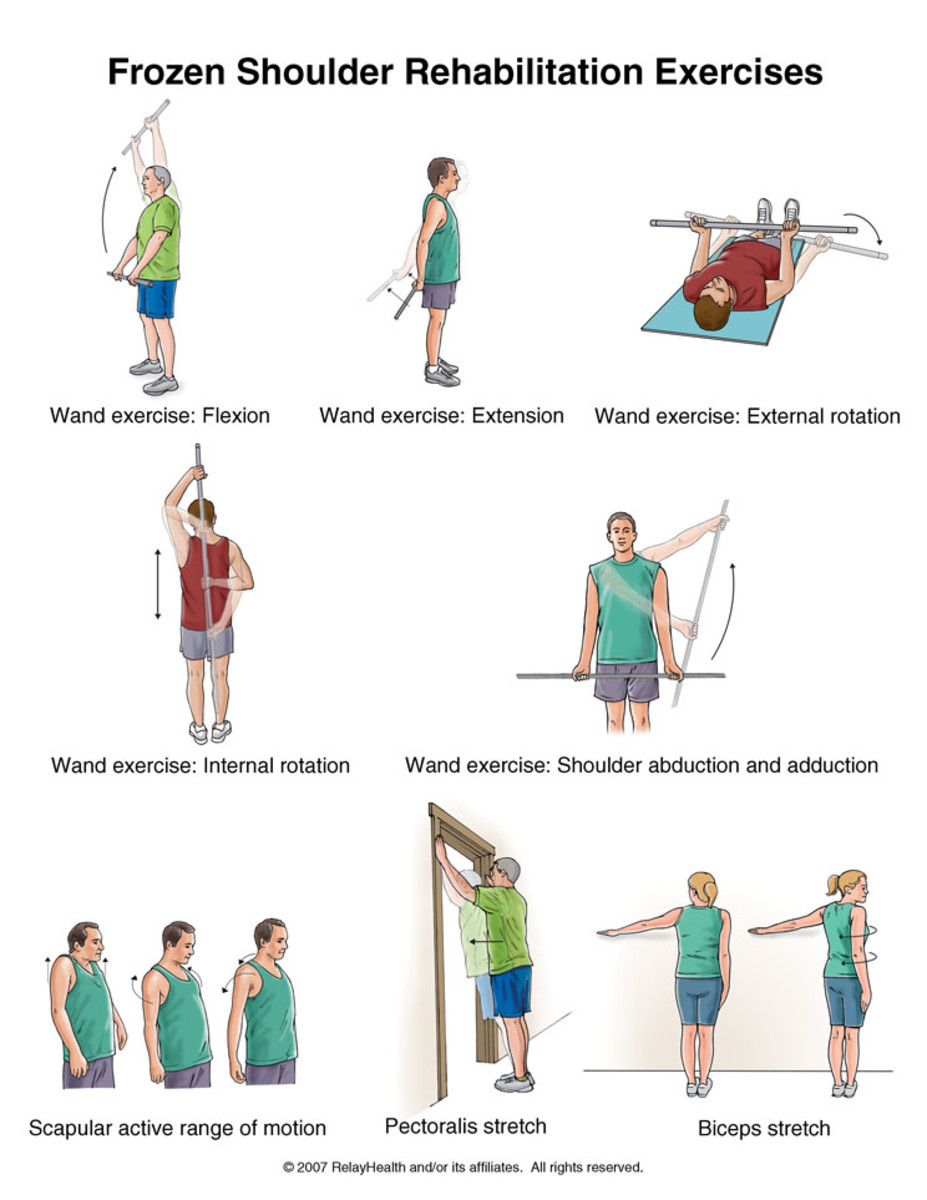
Example of exercise and treatment



No comments:
Post a Comment